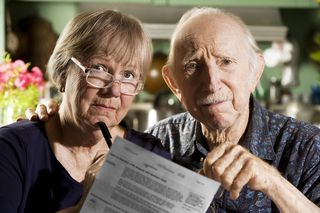
Higher fees are coming to high earners, when income thresholds for the highest surcharge tiers drop even further next year.
Higher fees are coming to high earners, when income thresholds for the highest surcharge tiers drop even further next year.
If you were hit with premium surcharges for Medicare Part B and Part D already, these costs will increase again in 2018, according to a recent article in Kiplinger, “Medicare Surcharge Thresholds to Drop.”
This recalibration of the trigger points was a part of the Medicare Access and CHIP Reauthorization Act of 2015, also called the "Doc Fix" law, which ended the annual battles over fee schedules for doctors' Medicare payments. To help pay for the permanent fix, lawmakers have asked high-income beneficiaries to foot the bill.
 Houston Estate Planning and Elder Law Attorney Blog
Houston Estate Planning and Elder Law Attorney Blog